November is Prostate Cancer Awareness Month.
Prostate cancer is the most commonly diagnosed cancer in Canadian men [1].
Starting at age 50, men are screened for prostate cancer regularly via a digital rectal examination (DRE). A DRE may also be done if men (regardless of age) experience urinary symptoms such as urgency, frequency, incontinence, dribbling, weak flow, pain on urination, blood in the urine, and/or other symptoms such as erectile dysfunction, painful ejaculation, swollen lymph nodes, chronic low back or pelvic pain, and weight loss. Laboratory testing of PSA (prostate-specific antigen) can also be used during the screening process and is used to monitor cancer progression; however, PSA is not specific to prostate cancer and can also be high due to benign prostatic hypertrophy, prostate infection and/or inflammation.
If any of the above screening measures are abnormal, a transrectal-guided biopsy of the prostate gland is conducted, and is the standard method of diagnosing prostate cancer. The results of the biopsy, as well as the PSA levels, will be used to determine the stage of disease, which is then used to determine monitoring/treatments.
Prostate cancer, unlike the majority of other cancers common in North America, tends to be slow-growing, with a high five-year survival rate (97.8%) [2]. Patient with low-risk disease are usually recommended to undergo ‘active surveillance’, which is monitoring of changes in symptoms and laboratory markers for cancer progression (ie. PSA, DRE) every 6-12 months before any treatment is recommended. This can be an incredibly stressful time for many, however there are various ways in which patients can take an active role in promoting beneficial changes to their health.
One of the ways in which people can promote healthy changes is understanding modifiable risk factors - these are various factors that influence the risk of developing prostate cancer that can be changed, unlike non-modifiable risk factors (such as age) [3, 4, 5]. Some risk factors for prostate cancer include:
Non-modifiable
Age (risk of prostate cancer increases as we age)
Having a first-degree family member with prostate cancer (ie. a father or a brother)
Ethnicity - black men are more commonly affected compared to white, Hispanic and Asian men
Various genetic mutations
Chemical exposures (e.g. Agent Orange)
A history of sexually transmitted infections
Modifiable
Being overweight or obese
A diet high in red meat and saturated fat
Lack of physical activity/exercise
Low blood levels of vitamin D3
Smoking
How can we modify our risk factors? Here’s a few examples:
Exercise: A 2015 study found that men with localized prostate cancer who engaged in walking/bicycling for at least 20 minutes per day had lower overall mortality rates compared to men who were less physically active [6].
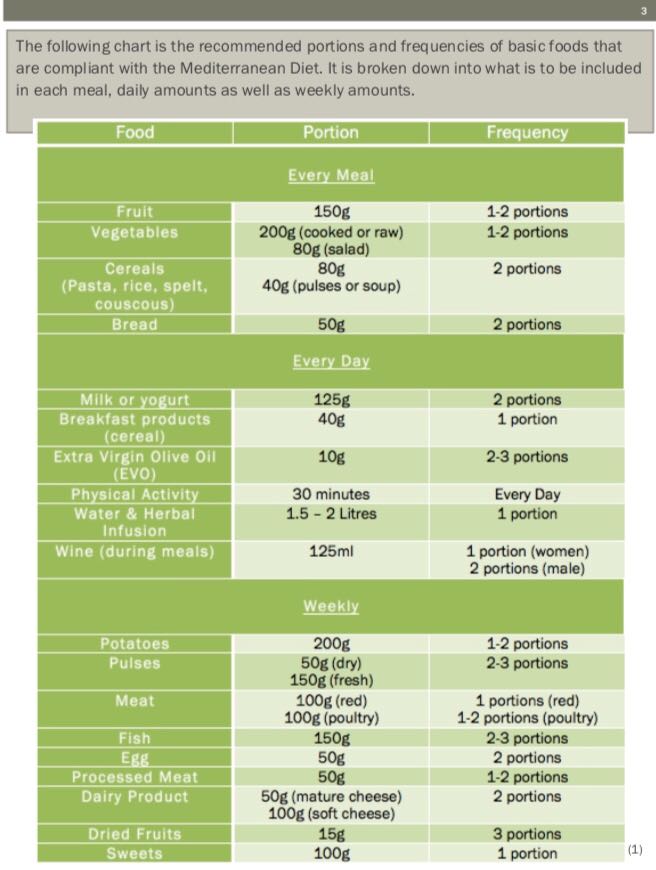
Diet: A 2014 study on more than 47000 men found that there was a 22% lower risk of overall mortality in men who ate a Mediterranean-style diet after their prostate cancer diagnosis [7].
Naturopathic medicine can be a useful addition to a person’s health care regimen. Naturopathic doctors (NDs) are well-trained to optimize diet, lifestyle, and nutritional status and implement evidence-based therapies that support overall health and emphasize disease prevention. NDs help guide patients toward making healthy changes and reducing their risk factors for disease.
Book a consultation today to find out how naturopathic medicine can support you!
Written by Dr. Dana Kolenich ND
References:
[1] Canadian Cancer Statistics 2019
[2] https://seer.cancer.gov/statfacts/html/prost.html
[4] https://www.ncbi.nlm.nih.gov/books/NBK470550/
[5] https://www.wcrf.org/dietandcancer/prostate-cancer
[6] https://cebp.aacrjournals.org/content/24/1/57
[7] https://pubmed.ncbi.nlm.nih.gov/23962747/