Breast health is a vital aspect of overall well-being for women of all ages. Did you know that breast cancer is the second-most diagnosed cancer in Canada and is the second leading cause of death among Canadian women over 50?[i] This October, as we honor Breast Cancer Awareness Month, we want to empower you to take proactive steps towards your breast health – because it’s never too early to start.
At Saskatoon Naturopathic Medicine, we believe in supporting you with an individualized approach looking at the body’s weaknesses and vulnerabilities that may make you susceptible to disease. Through optimizing nutrition, addressing environmental factors, or supporting your body’s natural defenses, we are committed to providing comprehensive care that treats the whole person.
Know the Risk Factors
Several factors can influence your risk of developing breast cancer. Some are within your control, while others – like family history or genetics – are not. Here are some key considerations:
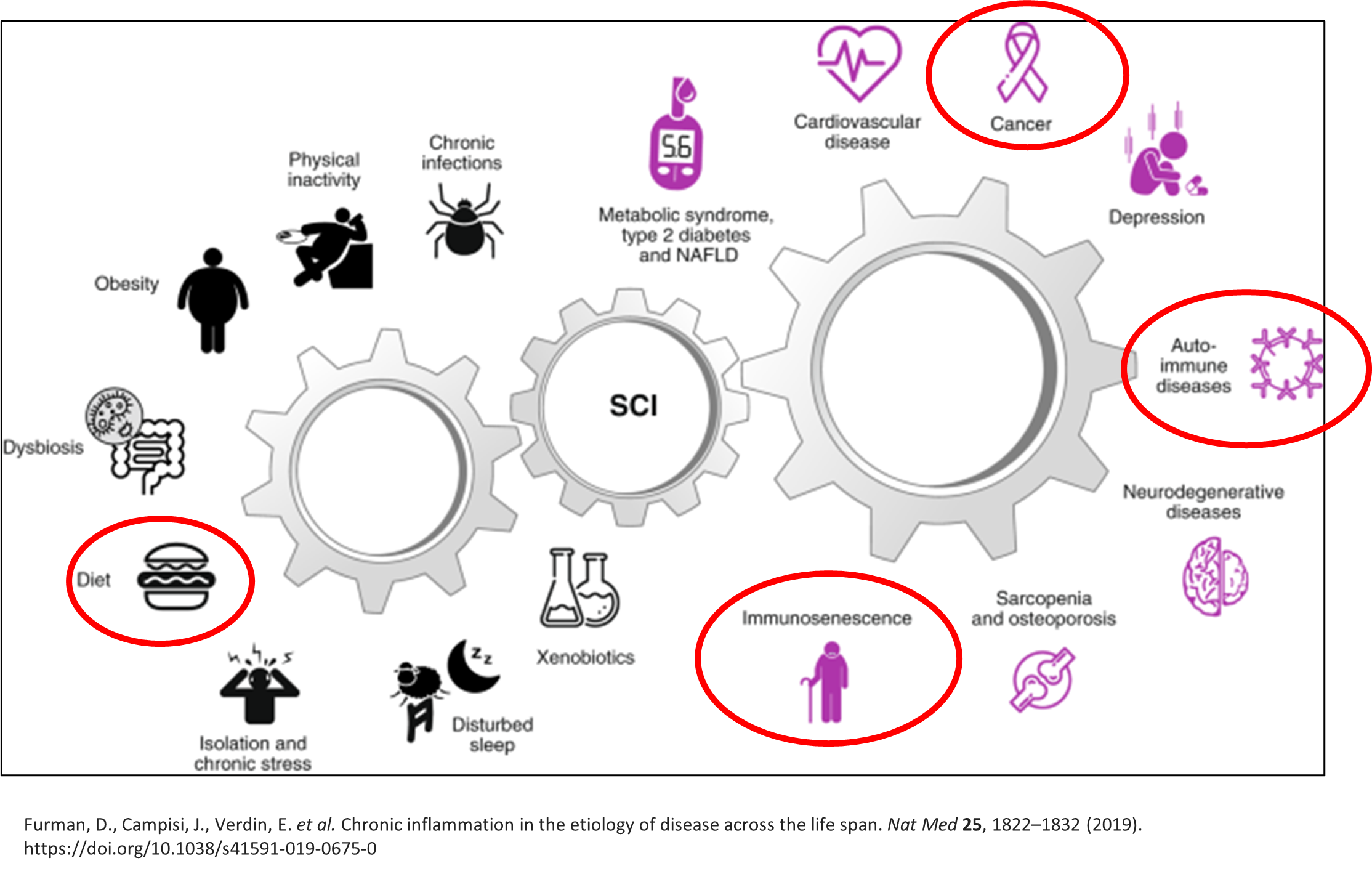
Nutrition : A balanced diet plays an essential role in reducing risks. Not only can a healthy diet directly improve our health, but it can also positively interact with many other factors involved in health like inflammation, body weight, hormone levels, and our gut microbiome. It is estimated that 30%-50% of cancers can be prevented through dietary changes.[ii] [iii] [iv]
Exercise and healthy lifestyle: Lack of exercise contributes to obesity, which in itself is a risk factor for breast cancer. In breast cancer patients, physical activity - both before and after the cancer diagnosis - has been associated with a lower risk of disease recurrence and reduced overall cancer-specific mortality compared to their sedentary counterparts. [v]
Family history and genetics: Understanding your genetic predispositions can guide proactive prevention.
Environmental toxins: Exposure to harmful chemicals (including alcohol and tobacco) can contribute to increased risk.
Dense breast tissue: Dense breasts not only elevate cancer risk but also make it difficult for cancerous lesions to be seen on a mammogram.
Being informed about these factors helps you take charge of your health, empowering you to make choices that align with your long-term wellness goals. Naturopathic doctors can break down these risk factors further to help you understand your vulnerabilities and strategize an individualized prevention plan.
Symptoms to Watch For
Breast cancer can manifest in various ways, some of which may be subtle. If you notice any of the following symptoms, it’s important to reach out to your healthcare provider for further evaluation:
Changes in breast size, shape, or appearance
New lumps, nodules, or cysts
Nipple discharge when not breastfeeding
Redness, pitting, or dimpling of the skin
Peeling or flaking of the nipple
Inverted nipples
Understanding Dense Breasts
Breast density[vi] is not about how your breasts look or feel – it is about tissue. Dense breasts have more glandular and fibrous tissue, making it harder for mammograms to detect cancer. However, having dense breasts is quite common, particularly in younger women. As women get older, their breasts typically become fattier and less dense (but this isn’t always the case). It is important to know your breast density so you can understand the risks and complications and make informed screening decisions.[vii]
You can learn more at www.densebreastscanada.ca.
Screening: Early Detection Saves Lives
Early detection is crucial, and regular screening is an important part of taking care of your breast health. As of January 2025, you will be able to self-refer for a mammogram in Saskatchewan beginning at the age of 40 (currently, the minimum screening age is 50).[viii]
Read that again – you do not need a doctor’s referral to make an appointment for a screening mammogram!
Just call 1-855-584-8228 to book your screening through the Screening Program for Breast Cancer. With screening centres throughout Saskatchewan (including a mobile unit that serves rural and northern Saskatchewan) accessing this potentially life-saving service is available to you.
How We Can Help
We are dedicated to helping you navigate these complex factors, providing tailored recommendations that fit your unique situation. Whether you are seeking prevention or already managing a diagnosis, our collaborative model works alongside conventional approaches to give you the best outcomes. From optimizing your nutrition and lifestyle to helping you understand your risks, we’re here to empower you at every step of your health journey, You deserve to feel confident, supported, and in control of your health.
[i] https://cancer.ca/en/cancer-information/cancer-types/breast/statistics
[ii] Mentella MC, Scaldaferri F, Ricci C, Gasbarrini A, Miggiano GAD. Cancer and Mediterranean Diet: A Review. Nutrients. 2019; 11(9):2059. https://doi.org/10.3390/nu11092059
[iii] Monllor-Tormos A, García-Vigara A, Morgan O, García-Pérez MÁ, Mendoza N, Tarín JJ, Cano A. Mediterranean diet for cancer prevention and survivorship. Maturitas. 2023 Dec;178:107841. doi: 10.1016/j.maturitas.2023.107841. Epub 2023 Aug 24. PMID: 37660598.
[iv] Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012 Jul-Aug;62(4):243-74. doi: 10.3322/caac.21142. Epub 2012 Apr 26. Erratum in: CA Cancer J Clin. 2013 May;63(3):215. PMID: 22539238.
[v] Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, Keadle SK, Arem H, Berrington de Gonzalez A, Hartge P, Adami HO, Blair CK, Borch KB, Boyd E, Check DP, Fournier A, Freedman ND, Gunter M, Johannson M, Khaw KT, Linet MS, Orsini N, Park Y, Riboli E, Robien K, Schairer C, Sesso H, Spriggs M, Van Dusen R, Wolk A, Matthews CE, Patel AV. Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern Med. 2016 Jun 1;176(6):816-25. doi: 10.1001/jamainternmed.2016.1548. PMID: 27183032; PMCID: PMC5812009.
[vi] https://cancer.ca/en/treatments/tests-and-procedures/mammography/breast-density
[vii] https://densebreastscanada.ca/faq/
[viii] https://densebreastscanada.ca/breast-cancer-screening-in-saskatchewan/