Have you been told you have a “fatty liver” despite not consuming high amounts of alcohol? If so, you have NAFLD or NASH.
What is NASH/NAFLD?
>> Nonalcoholic Fatty Liver Disease (NAFLD, Hepatic Steatosis, NASH)
Non-alcoholic fatty liver disease (NAFLD) is a chronic and multifactorial disorder characterized by excessive fatty acid accumulation in liver cells. Associated with metabolic syndromes, NAFLD is increasingly being recognized as a major cause of liver disease. It is a spectrum of liver abnormalities that ranges from nonalcoholic fatty liver to steatohepatitis, cirrhosis, and liver cancer. It is estimated that 25% of the global population has NAFLD, a number projected to continue to rise, and as it does, it is expected that more of these cases will progress to end-stage disease states requiring liver transplantation. A larger percentage of liver cancers in these cases occur before end-stage liver failure, and thus are less likely to be screened for, increasing the tendencies for liver tumors to be larger and more difficult to treat at the time they are diagnosed. Testing and diagnosis of NAFLD may include blood tests, imaging, and biopsy.
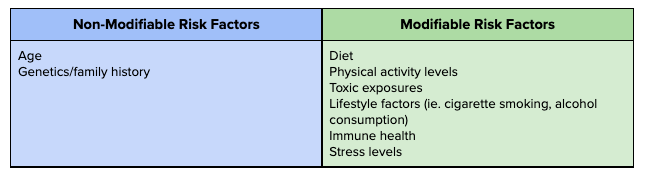
What causes it?
Risk Factors
• Metabolic syndrome (strongest risk factor)
increased waist circumference (obesity)
insulin resistance
elevations in:
blood sugar
cholesterol
triglycerides
blood pressure
uric acid
• Diabetes (up to 75% of individuals with type 2 diabetes have NAFLD)
• Sleep apnea
• Gut microbiome effects
• Genetic factors
Image: Friedman et al. 2018
Why is it important to address?
Patients with NAFLD are twice as likely to die of cardiovascular disease than liver disease as a result of these shared risk factors. NAFLD in itself is an independent risk factor for cardiovascular disease due to its impacts on vascular health and inflammation.
How does it happen & what you can do about it?
Free fatty acids from either adipose tissue (fat), or from the conversion of excess carbohydrate intake, accumulate in the liver cell resulting in oxidative stress, inflammation, and liver injury.
As such, healthy eating habits and regular exercise can reduce the amount of free fatty acids and thereby prevent or reverse NAFLD. Glutathione supplementation can also help in the recovery of NASH/NAFLD.
What is Glutathione?
Glutathione (GSH) is a tripeptide made from amino acids, that is present in every cell of the human body, though is highly concentrated in the liver. Known as the ‘master antioxidant’ it directly scavenges reactive oxygen species, protecting your body from oxidative damage, and plays a crucial role in detoxification and cellular health. Reduced levels of glutathione have been associated with increased disease risk and progression, including NAFLD and other liver pathologies.
In addition to healthy diet and lifestyle habits, preliminary studies have shown beneficial effects of supplemental glutathione in the treatment of NAFLD, demonstrating a reduction of ALT–a liver enzyme elevated in liver dysfunction and one of the principal NAFLD biomarkers–after four months of treatment. Other studies demonstrated intravenous glutathione rapidly improved liver function, also evidenced by reduced biomarkers, in the treatment of other liver pathologies including chronic hepatitis B. Various nutrients, amino acids, herbal extracts, and probiotics have also been shown to increase glutathione activity in the body, and may be used in conjunction for enhanced therapeutic effect.
Find out if Glutathione is an option for you!
At Saskatoon Naturopathic Medicine, we offer both oral and intravenous glutathione for the treatment of NAFLD and other conditions, as part of our comprehensive approach to our patients’ unique health history and needs. If you are interested in learning more about how we can assist you, give us a call or book online to connect with one of our naturopathic doctors who would be happy to assess your case and discuss treatment options appropriate for you.
*IV therapy requires a consultation and evaluation by one of our IV doctors to assess patient eligibility and treatment goals. For more information see our IV therapy page.
Jacalyn Sieben, ND
Sources:
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M., & Sanyal, A. J. (2018). Mechanisms of NAFLD development and therapeutic strategies. Nature medicine, 24(7), 908–922. https://doi.org/10.1038/s41591-018-0104-9
Honda et al. (2017). Efficacy of glutathione for the treatment of nonalcoholic fatty liver disease: an open-label, single-arm, multicenter, pilot study. BMC Gastroenterology. 17:96 DOI 10.1186/s12876-017-0652-3. https://pubmed.ncbi.nlm.nih.gov/28789631/
Vairetti, M., Di Pasqua, L. G., Cagna, M., Richelmi, P., Ferrigno, A., & Berardo, C. (2021). Changes in Glutathione Content in Liver Diseases: An Update. Antioxidants, 10(3), 364. MDPI AG. Retrieved from http://dx.doi.org/10.3390/antiox10030364
Qian, L., Wang, W., Zhou, Y., & Ma, J. (2017). Effects of reduced glutathione therapy on chronic hepatitis B. Central-European journal of immunology, 42(1), 97–100. https://doi.org/10.5114/ceji.2016.65894